Antonia Hylton is a Peabody and two-time Emmy award-winning Correspondent for NBC News and MSNBC and the cohost of the hit podcasts Southlake and Grapevine. She was formerly a correspondent and producer for Vice News Tonight. Since 2019, she has also served as an annual judge for the American Mosaic Journalism Prize. Antonia graduated magna cum laude from Harvard University in 2015, where she received prizes for her writing and investigative research on race, mass incarceration, and the history of psychiatry.
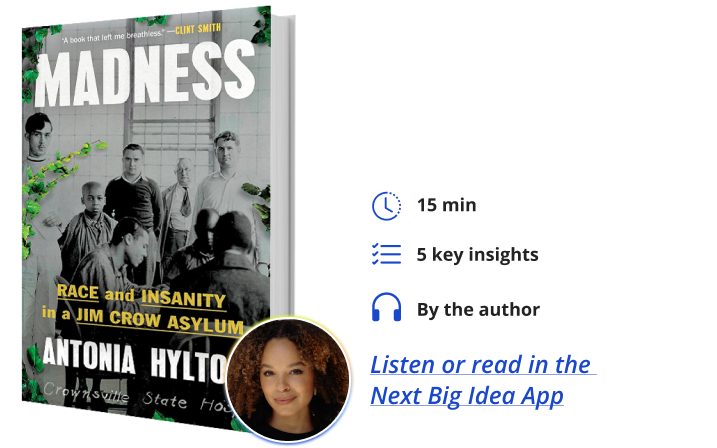
Below, Antonia shares 5 key insights from her new book, Madness: Race and Insanity in a Jim Crow Asylum. Listen to the audio version—read by Antonia herself—in the Next Big Idea App.
1. History and culture shape mental health.
Like every field of medicine, psychiatry did not develop in a vacuum. The prevailing beliefs, attitudes, and power structures at any place and point in time shape the way we view and treat mental illness. For Black Americans, this means that for many decades, white physicians and administrators at hospitals viewed them as inferior and different. In the mid-19th century, one physician and researcher named Samuel Cartwright came up with a mental disorder he called “Drapetomania,” used to describe Black people who tried to flee the control of their masters. He and many of his colleagues believed Black people were lazy, immoral, and unable to mentally withstand the responsibility of being free. Rarely did doctors consider the role that enslavement might have played in those patients’ suffering.
These attitudes directly influenced psychiatric practice and the services made available (or unavailable) to certain communities. The belief that Black people’s mental wellbeing required constant, hard labor led doctors to segregate white and Black patients into separate wards or hospitals, and subject Black patients to more forced labor and agricultural work at those same hospitals than white patients. Crownsville Hospital, originally called Maryland’s Hospital for the Negro Insane, was one such institution. The very first patients committed to the hospital were the only patients ever forced to do the back-breaking work of building their own asylum from the ground up.
2. Outsiders drive innovation.
Outsiders are often the only people who can see an institution—like a sprawling hospital—for what it truly is. The arrival of just one or two people who have a different vision and who are less afraid of change can have the power to reset the course of history.
For decades, Crownsville Hospital was led by Dr. Robert Winterode, the same physician and superintendent present at the hospital’s founding in 1911. Patients and families connected to the hospital often feared and despised him for forcing the patients to work, allowing the hospital’s conditions to deteriorate, and for refusing to hire any non-white people as employees.
“Having narrowly escaped the Nazis, Dr. Morgenstern became extremely uncomfortable with the antebellum and racist practices of the hospital.”
But in the 1940s, a Jewish doctor and Holocaust survivor by the name of Dr. Jacob Morgenstern arrived. Having narrowly escaped the Nazis, Dr. Morgenstern became extremely uncomfortable with the antebellum and racist practices of the hospital. He began to invite patients to spend time with his family and fight for new medications and therapies. He eventually took over as Crownsville’s leader. It was his outsider status—his lack of reverence for southern “tradition” and lack of fear of the political elite in Maryland—that roused him to desegregate the hospital and onboard Black employees for the first time.
Dr. Morgenstern developed a friendship and alliance with a Black doctor named Vernon Sparks, who then created a prestigious training pipeline for aspiring psychologists and psychiatrists. To this day, many Black doctors in Maryland credit Sparks as an inspiration and say they were able to benefit from the programs he created.
3. For some, “deinstitutionalization” was a “reinstitutionalization.”
When we talk about deinstitutionalization or the shuttering of asylums and mental hospitals around the country, we often think of a very simple story. That story goes something like this: Americans learned about the horrors going on inside the asylums that were once all over the country, and our increased empathy and understanding for people living with mental illness combined with the arrival of new medications in the 1950s and 1960s rendered these institutions unnecessary.
The truth is much more complicated than that, especially in communities of color. At the very same moment that our culture became more sympathetic to people living with mental or emotional challenges, it also began to invest in an expanded criminal justice system that tended to target poor people and communities of color. During this period in the second half of the 20th century, doctors at Crownsville observed and reported that their patients were increasingly likely to land in jail or prison after leaving the hospital. So while some patients benefited from a new ethos of care and compassion, others were quickly re-institutionalized elsewhere. All of these shifts are connected.
4. Community is the key to recovery.
Medication and therapy alone often aren’t enough to heal mental suffering. People desperately need community. In my decade of research and interviews with patients and practitioners, I’ve found a clear pattern: the patients who have made the most powerful recoveries have been surrounded by people and neighbors who love them unconditionally and show up for them consistently.
“People desperately need community.”
This is one of the most glaring challenges facing our mental healthcare system today. Although our politicians once promised that they would build community mental health centers and clinics in every state, very few of those sites have materialized.
Dr. Tami Benton, psychiatrist-in-chief at the Children’s Hospital of Philadelphia, once told me that the children she serves live with extreme uncertainty and consistently report that they believe our society is failing them. According to her research, less than half of Black children who come to emergency rooms in the midst of a mental health crisis are able to connect to ongoing care and support after the visit. This absence of community, safety, and dependability is driving an increase in youth suicides. Many doctors believe it is jeopardizing our collective future.
5. Talk (or write) about your grief.
This one is a little personal. But one of the greatest lessons of my research is this: pain demands your attention, and one way or another, it will catch up with you. The more we talk about depression, anxiety, and grief, the easier it is to find a supportive community and move forward. It can save lives. In the same way that many of us want to know our family history of cancer or diabetes, we need to know our family histories of mental illness. There is still so much about the origin and biological causes of mental illness that doctors do not know. What they do know is that early detection and early intervention are the best tools that we have. Early detection is only possible when families release stigma and talk.
As I was writing, I helped take care of a loved one who was in the midst of a psychiatric crisis. We would go on walks together, and they would tell me everything they were going through. I did my best, in turn, to help them communicate with doctors. I also shared my reporting with them and incorporated their advice and insights. These walks and visits helped us weather the long storm and ultimately helped our family find the other side.
To listen to the audio version read by author Antonia Hylton, download the Next Big Idea App today:































