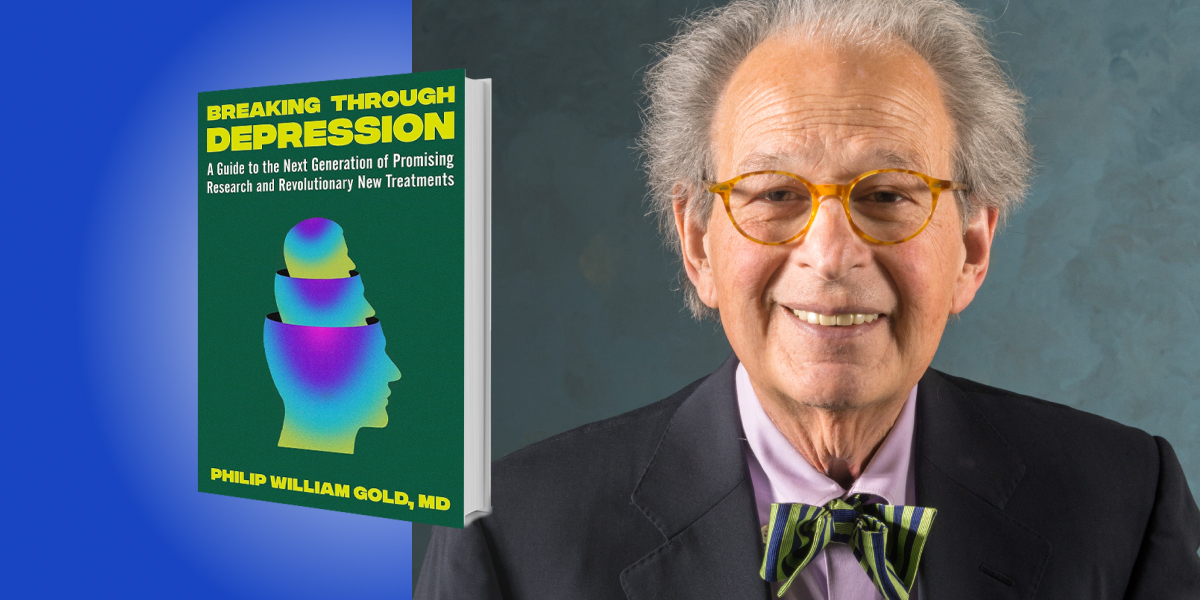
Dr. Philip William Gold has been a laboratory chief at the NIH Clinical Center and has spent the last 48 years there studying the neurobiological basis of depressive illness. He has written over 400 scientific articles that have been quoted by over 65,000 other publications. He was appointed to the 14-member Library of Congress Council of Scholars and has participated in the MacArthur Foundation Medical Network. He has won numerous national and international prizes for his research and delivered honorary lectures at institutions such as Harvard University and the Japan Foundation.
Below, Dr. Gold shares five key insights from his new book, Breaking Through Depression: A Guide to the Next Generation of Promising Research and Revolutionary New Treatments. Listen to the audio version—read by Dr. Gold himself—in the Next Big Idea App.
1. The evolution in my thinking about depressive illness.
My thinking about depression goes back to over 60 years ago. As a college student in the late 1960s, I majored in English. When I decided to go on to medical school, I did so with the intention of training in psychiatry. My wish to study psychiatry reflected a belief that it represented a form of applied literature, where what I came to understand about the world could be expressed therapeutically. What good was our knowledge, I wondered, if we couldn’t help someone who had lost the will to live to find a way back into the world? Even if I would never understand the meaning of life, I knew that pain mattered, we all experience pain, and that a purposeful and worthy goal is to attempt its alleviation. For these reasons, I pursued psychotherapy for the treatment of depression.
As I sought to help my patients work through their struggles with depressive illness, it became increasingly clear that although depression was related to painful memories and stressors, there were biological factors as well. Data was emerging indicating that there are genetic components to depression. We also knew then that hormonal disturbances could trigger depressive episodes, which resolved when the hormonal disturbances were corrected. Moreover, cyclical patterns of depressive episodes seemed to involve alterations in biological rhythms. I saw that if I were going to truly understand what depression was about, I needed to learn more about these underlying biological changes.
2. The biological foundations of depression.
Recent research has revealed exciting data that revolutionizes our understanding of the pathologic brain mechanisms that are responsible for depressive illness. This research has led to the development of a new generation of rapid-acting antidepressants that work within hours, rather than weeks, in depressed patients to ameliorate structural brain abnormalities and multiple other biological deficits.
“There is a marked reduction in the birth of new neurons which promote the capacity to deal with complex, shifting environmental stressors.”
While this is certainly good news, the bad news is that depression is a far worse illness than we had previously suspected. It is not only associated with widespread damage and destruction of brain cells that encode identity, self-esteem, and other key aspects of our humanity but also by inflammation in the brain and throughout the body. Neurons in depressed individuals fail to properly connect to one another and there is a marked reduction in the birth of new neurons which promote the capacity to deal with complex, shifting environmental stressors. In addition, synapses, or the spaces that bridge nerve cells through which neurons communicate, are damaged and decreased in number. Moreover, neuronal pathways become atrophied and malfunction.
3. The two major clinical forms of depressive illness.
The first major form of depressive illness is melancholic depression. Loss of self-esteem and feelings of worthlessness are particularly tragic behavioral features of this depressive syndrome, which affects 30-35 percent of patients with depressive illness. Melancholic depression contradicts the meaning of depression as a suppression of thought and feeling. Rather, it is often associated with anxiety, especially directed at the self, hyperarousal, increased vigilance, and bombardment and retrieval of a host of painful negatively charged emotional memories of loss and failure that help define the agonized mood of melancholia. Melancholic depression is also associated with loss of the capacity to anticipate or experience pleasure, and an increased expectation of harm. I conceptualize these symptoms as a cancer of the self.
One of the key sites of neuronal pathology is the subgenual prefrontal cortex, which loses as much as 40 percent of its volume and much of its function. This site modulates self-esteem, anxiety, the capacity to experience pleasure, multiple hormonal systems, and the sympathetic nervous system. Accordingly, individuals with melancholic depression are beset by the dysregulation of multiple hormone systems and metabolic functions. They also have increased inflammation, increased blood clotting, and increased levels of blood sugar levels to deal with the danger at hand and to preemptively protect them from possible injuries incurred in fight situations. These changes also occur during psychological stress such as public speaking. Melancholic patients characteristically have insomnia, often manifested as early morning awakening, and loss of appetite, with weight loss. A depressed mood is often more severe in the morning than in the evening.
“Melancholic depression is also associated with loss of the capacity to anticipate or experience pleasure.”
The second major form of depressive illness is atypical depression. We know less about this form of depression, which affects approximately 30 percent of depressed individuals. Atypical depression seems the antithesis of melancholia. Instead of an activated state associated with a bombardment of negatively charged emotional memories, patients with atypical depression feel remote from themselves, others, and their pasts. They experience chronic fatigue, loss of motivation, increased sleep, and increased appetite, and often gain weight. Depressed mood is more severe in the evening than in the morning. Individuals with atypical depression fail to respond to some drugs that are effective in melancholia.
4. Depression is a total-body disease.
Depression doesn’t just affect the brain and nervous system. Many brain-driven hormonal changes, as well as inflammation and sympathetic nervous system activation, lead to abnormalities in growth, reproduction, immune responses, metabolism, and tissue repair. The heart, blood vessels, bone, muscle, fat, and connective tissues suffer damage, leading to the premature onset of coronary artery disease, stroke, diabetes, and osteoporosis. All of this adds up to theft of 7 to 10 years of life, independent of smoking, hypertension, or suicide. Accordingly, the World Health Organization has declared that depression is the second greatest cause of disability worldwide.
5. Depression represents a dysregulation of the brain’s stress response system.
In the hyperarousal of melancholia, the stress system is distorted and pathologically activated. In the chronic fatigue, increased sleep, and the distance from self and others that characterize atypical depression, the stress system is suppressed. Stress alters the structure and function of the prefrontal cortex, the emotion-generating areas of the brain, and areas that encode identity and self-esteem. Because the stress system is the area that is principally affected in depression, psychotherapy is essential as an adjunct to medication in the effective treatment of depressive illness. Otherwise, environmentally-mediated residual conflicts and maladaptive behaviors are likely to override the effects of otherwise successful antidepressant treatment.
“Often, within hours, they ameliorate many of the structural and physiological abnormalities in depressive illness.”
A new generation of as many as 30 rapid-acting antidepressants is emerging based on new concepts regarding the biology of depressive illness. Often, within hours, they ameliorate many of the structural and physiological abnormalities in depressive illness. Some of these, like ketamine, are already available. Others, like psilocybin, have completed clinical trials and will soon be available. Anti-inflammatory drugs and those that promote the birth of new neurons or enhance connections among neurons are also effective, even in otherwise treatment-resistant depression. These drugs far exceed the capacities of SSRI’s and even older antidepressants which have held sway for over 50 years.
I would like to emphasize that in contrast to the years 1960 to 2000, when progress in biological psychiatry was slow and there were only a small handful of effective antidepressants, we have recently identified multiple new targets in the brain for antidepressants. Over 30 new compounds are in clinical trials and in basic science studies. I have tried to illustrate that even though depression is a thoroughly biologically mediated disease, it is the stress system in the brain that is primarily affected. Since stress alters the structure and function of the stress system, psychotherapy is essential for the optimal treatment of depression. Depression affects much of the brain and widespread hormonal and autonomic systems in a way that shortens life, so it fully deserves to be covered by insurance plans that cover other severe illnesses. I hope that this book adds to the growing awareness that depression is not a sign of weakness or inadequacy, but rather an illness beyond our control, and that surviving it takes courage, determination, and the capacity to bear enormous pain.
To listen to the audio version read by author Philip William Gold, download the Next Big Idea App today: