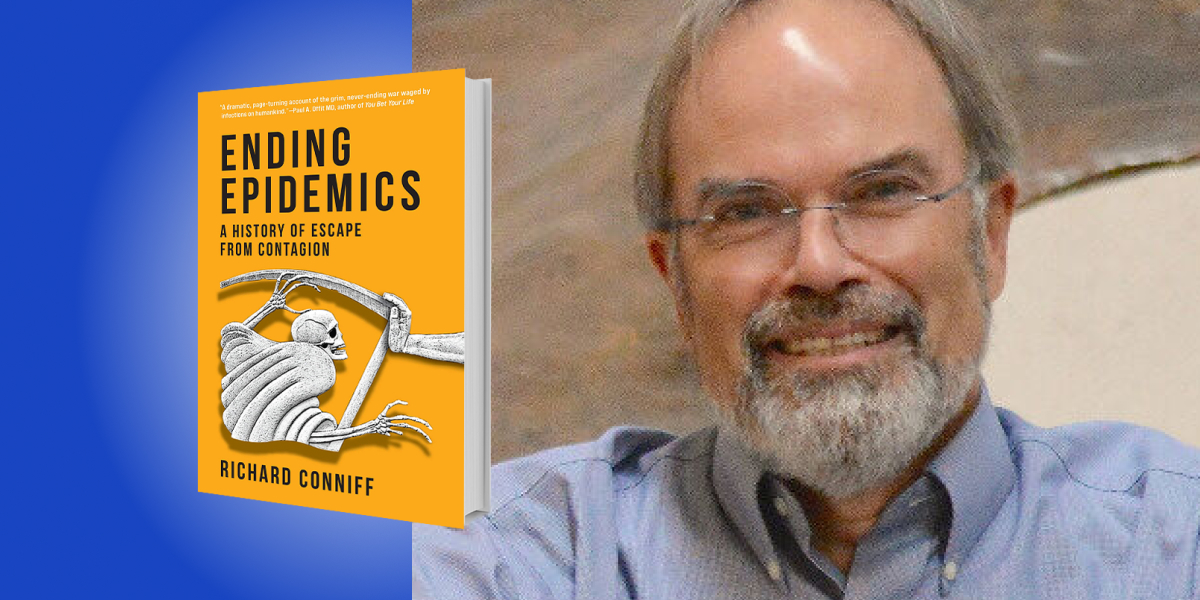
Richard Conniff is an award-winning nonfiction writer. He specializes in the topics of human and animal behavior, with his work appearing in the New York Times, Smithsonian, The Atlantic, and National Geographic, among others.
Below, Richard shares five key insights from his new book, Ending Epidemics: A History of Escape from Contagion. Listen to the audio version—read by Richard himself—in the Next Big Idea App.
1. Public health is a personal story for all of us, and we take it entirely for granted.
Just ask an uncle or a grandmother what kind of diseases they grew up with. In my family, for instance, my father and uncle both had polio as toddlers in the 1920s. My uncle got it worse, with legs that were permanently reduced to sticks. He spent the rest of his life walking with the help of arm braces.
Summer was still polio season when I was a toddler. At that time, polio was annually killing more than 3100 people in this country and paralyzing 21,000. But in 1955, Jonas Salk’s polio vaccine became available and people flocked to get it. I was one of them. “Polio season” could now just be called summertime.
Progress against infectious disease accelerated from there. My own kids avoided almost all the childhood diseases that were routine for me. A major international effort also began knocking down childhood diseases, with polio, for instance, eliminated from all but two nations by 2019. Now, kids my grandson’s age are being protected against diseases most parents never heard of, like rotavirus, which used to routinely kill small children.
Think about that. If you had told someone 150 years ago that human ingenuity and effort could eradicate smallpox everywhere, forever, and largely eliminate a murderer’s row of childhood diseases, they would have said it couldn’t be done. If you told them that improvements in public health would double the average human life expectancy in less than a century, they would have said again that couldn’t be done.
Yet it happened and is the single most dramatic change in human history. But to say it happened within living memory is wrong. There is a Catch-22 to vaccines, antibiotics, and all infectious disease prevention measures: they save us from diseases, but then cause us to forget about the diseases from which they have saved us.
Our sense of freedom from all the diseases that haunted our parents and grandparents has given us the bizarre sense that we are somehow naturally immune—and no longer need to take basic precautions. We need to remember how incredibly far we have come, and how we got here, to have a chance of facing down the epidemics that still lie ahead.
2. Medical discovery isn’t a story about a few big names.
Let’s start with one of the biggest. Jonas Salk was practically a saint when I was a kid. In fact, I still have my vaccination certificate from the first year of the Salk vaccine. My parents kept it in a folder of sacred documents, together with my baptismal certificate.
“New ideas don’t spring up out of nowhere and instantly change everything.”
But no great discovery is ever the unaided work of a lone genius or wholly original. New ideas don’t spring up out of nowhere and instantly change everything. They almost always result from collaboration among many researchers.
Most of their names get left out of the story. Isabel Morgan, for instance, faced predictable challenges in the mid-20th century workplace. The director of one institute she worked at described her as a brilliant young virologist and also “a very handsome-looking girl.” He added, “It’s just that I don’t think that she could have advanced very far at the Institute…few Ph.D. ladies ever had much of a chance for advancement at the Institute during the early days.”
Morgan moved on to Johns Hopkins University and by 1951 she had developed a formalin-inactivated polio vaccine (the prototype of the Salk vaccine) and she demonstrated that she could immunize experimental monkeys against all three types of poliovirus—everything needed to prevent polio except testing in humans.
But Morgan stopped there, maybe because she had married and married women back then weren’t supposed to work, or because she chose to care for a stepson with a learning disability, or maybe she shrank from the risky business of testing on human children. The March of Dimes, which paid for most polio research, was soon putting its money on Jonas Salk—and all the glory followed.
So maybe we shouldn’t call it the Salk vaccine, nor the Morgan vaccine, because that’s not how science works. Every great breakthrough builds on the prior work of countless others.
3. The fight against infectious disease isn’t only about great medical discoveries.
One of my favorite characters in Ending Epidemics was a social reformer named Edwin Chadwick. He campaigned aggressively in the 1840s and 50s for the British government to intervene in matters of public health. Chadwick wanted centralized systems of public water supply and sewerage. That work laid down the blueprint for making large modern cities livable.
He succeeded by undertaking a massive exploration of the lives of the urban poor. Then he explained what he saw in vivid detail to readers for whom the world just around the corner was as alien as the slums of Calcutta. His 1842 Sanitary Report, from the government’s own Stationery Office, has been called “a masterpiece of protest literature.” It sold 100,000 copies.
“That work laid down the blueprint for making large modern cities livable.”
Politicians balked at first. London’s Mayor declared that there could be no improvement to the water supply system because it was already perfect. Two years later, cholera was spread via that same water system, killing 15,000 residents.
Chadwick’s work ultimately led city governments in London and beyond to build municipal water supply systems and safer sewerage. By limiting the spread of cholera, typhoid, polio, and other water-borne diseases, those systems have saved lives and increased life expectancy. Continuing to extend the kind of sanitary reforms Chadwick pioneered throughout developing world cities today is probably the most important thing we can do to improve public health.
4. All vaccines involve risks and benefits.
For instance, the vaccine for HPV can cause pain where the shot was given. Fever, dizziness, and nausea can also occur. That’s the risk. These effects are almost always temporary, but misinformation about risk caused uptake of the vaccine in Japan to drop from 70 percent in 2013 to just 1 percent almost overnight. The scare didn’t spread to the United States, and a study this year found that for American women in their 20s, the HPV vaccine produced a 65 percent decline in cervical cancers. That’s the benefit.
In this country, plenty of parents worry about the MMR vaccine, for measles, mumps, and rubella. Part of the problem is that they never see measles anymore and imagine that it is a minor disease. It isn’t. I had measles in 1958 before a vaccine existed. I had it so bad my parents thought I was going to die—and 552 other American kids with measles did die that year. That’s in addition to the one in 1000 measles victims who suffer encephalitis, often resulting in permanent hearing loss or intellectual disability. One in 20 suffer pneumonia, the leading cause of measles deaths.
What parents worry about is an imaginary link between the MMR vaccine and autism. A link that was invented by a doctor working on a lawsuit against vaccine manufacturers. A link that has been repeatedly disproved, most recently in a study of more than 600,000 children.
Like every other vaccine, the MMR vaccine has risks. They can include febrile seizures, which sound bad, but that symptom is rare and typically without lasting effect. Being a good parent isn’t about protecting children from every possible risk. It’s about making a judgment, with advice from a doctor, about relative risk.
“Being a good parent isn’t about protecting children from every possible risk.”
Because so many parents made the wrong judgment about risk, almost 1,300 American children came down with measles in 2019. About 130 of them needed hospitalization, and 64 of them suffered complications including pneumonia and encephalitis. This was just two decades after public health officials proudly declared measles eliminated from North America.
5. History matters in preventing epidemics.
Some of the best lessons come from a public health effort that began almost by accident in 1966. That’s when the WHO, the World Health Organization, launched a campaign to eradicate smallpox worldwide. It was a wildly ambitious, ill-planned, and probably unreachable goal, and they meant to get it done in just 10 years.
But as the campaign got started in Brazil and Indonesia, that global ambition lit a fire under public health workers. Both countries soon freed themselves from this genuinely horrible disease. Experienced workers from those countries went on to teach other countries how to track down smallpox cases. They became part of a multinational team of public health workers, armed with the simplest technologies—a smallpox vaccine not so different from the first one developed in the 18th century and a bifurcated needle that had no moving parts.
It wasn’t just a story of international cooperation but also of heroic individual effort. Teams of vaccinators traveled in floods, droughts, famine, and civil war. There were no cell phones to call for help in emergencies. For instance, in Ethiopia, a helicopter pilot was kidnapped by rebels. He took the opportunity to vaccinate his captors.
Public health workers finally cornered the last known case of naturally acquired smallpox in Mogadishu in October 1977. The WHO campaign had missed its goal to eradicate smallpox in ten years, but just barely. An astonished observer remarked, “The workers in the program were simply too young to know it couldn’t be done.”
The lesson the WHO learned from all this was that vaccines work. It went on to increase uptake of six basic childhood vaccines from just 5 percent in the 1980s to 86 percent or better in almost all nations by 2019, with a corresponding decline in disease. We could expand that now to bring basic medical care, safe drinking water, and sanitation to the billions who lack these necessities for human health. We could eradicate other notorious diseases, like polio and measles. The world has become too small and moves too fast for us to waste time fighting one another. We need to accept that infectious diseases anywhere are now infectious diseases for all of us. Working together to stop them is the only way to protect ourselves from the epidemics that lie ahead.
To listen to the audio version read by author Richard Conniff, download the Next Big Idea App today: