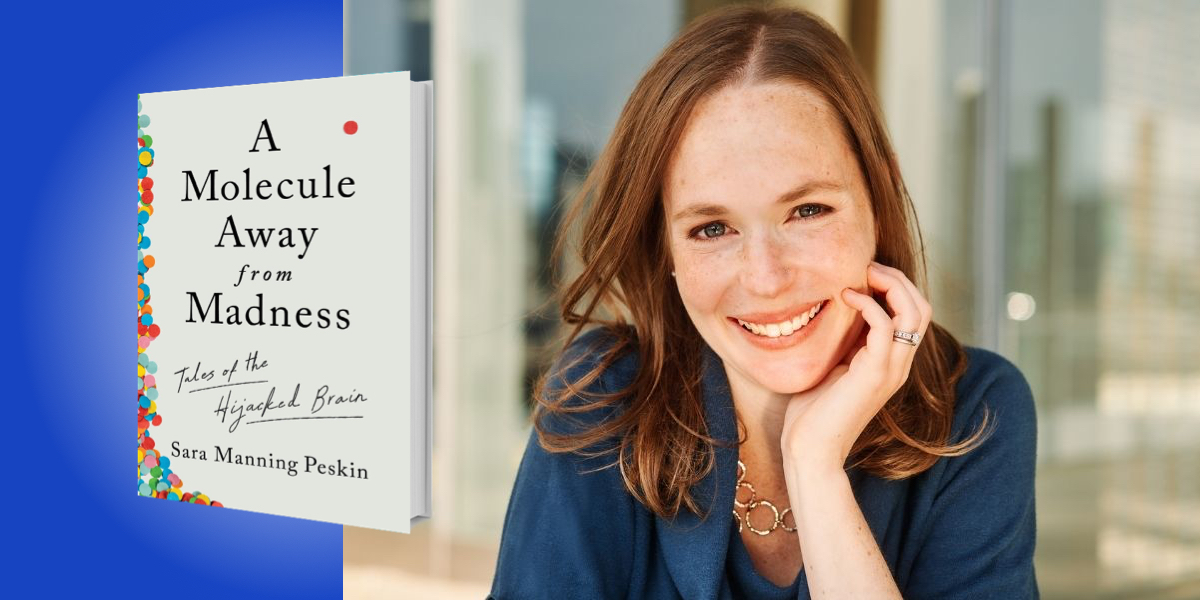
Sara Manning Peskin is a cognitive neurologist at the University of Pennsylvania. Her new book is about people whose personalities have been upended by single molecules, and about the scientists who work to bring patients back from the brink. Her writing can be found in the New York Times, Boston Globe Magazine, and the Philadelphia Inquirer.
Below, Sara shares 5 key insights from A Molecule Away from Madness: Tales of the Hijacked Brain. Listen to the audio version—read by Sara herself—in the Next Big Idea App.
1. Set up shop in the right place.
People used to think that the nervous system was made of a single, enormous mass, but Santiago Ramón y Cajal, a Spanish scientist, looked into his microscope in the late 1800s and discovered that the world was wrong. Instead, the brain is made of lots of individual cells—what we now call “neurons.” Ramón y Cajal recognized the importance of his finding, and spent much of his salary to send printed copies of his results to scientists around the world. Rumor has it that he spent so much money that he couldn’t afford a nanny, and even had trouble buying curtains.
Ramón y Cajal expected to receive a deluge of praise, but instead there was near silence. Going over the data, he realized that nobody was going to change their mind based on a piece of paper. So, he packed his slides and microscope and went off to Germany, where he set up a booth at a scientific conference. People lined up to look at his slides, and by the end of the conference, he convinced the giants in the field that the prevailing idea about the nervous system was wrong. The finding soon won him a Nobel Prize. Had he given up earlier, stayed at home, and not realized the importance of experiential learning, who knows how much longer we would have persisted with a fundamental flaw in our understanding of the nervous system. He was the ultimate go-getter, a person who knew how critical it was to keep trying.
2. Look up from your desk.
In the late 1800s, a researcher named Christiaan Eijkman set out to study multiple neuritis, a deadly disease that was causing droves of Dutch military personnel to become so weak that they couldn’t breathe. Eijkman thought the condition was caused by a toxin, but, one after another, his experiments failed to prove it.
“Eijkman began to wonder if the chickens might be suffering from the same disease as the Dutch soldiers.”
Nearby in the same laboratory, he noticed that a collection of chickens began to develop a disease similar to multiple neuritis. Out of nowhere, the birds became extraordinarily weak, keeling over on their wings and dying. Looking up from his own experiments, Eijkman began to wonder if the chickens might be suffering from the same disease as the Dutch soldiers.
But before he could do any experiments on the chickens, they magically returned to health. Eijkman’s mind quickly turned to the chicken’s diet. He found the laboratory keeper, who explained that a few months earlier, to save money, they began feeding the chickens leftover white rice from the cafeteria. The chickens had gotten sick not long after this. Later in the fall, a new chef had come on base and refused to give military rice to civilian chickens. So, the chickens began eating brown rice again, and the disease had soon disappeared.
With impressive speed for a government endeavor, Eijkman organized a massive trial to test whether brown rice prevented multiple neuritis—and it did. Scientists went on to discover that brown rice contains high levels of thiamine, also known as vitamin B1. Multiple neuritis became a preventable, treatable disease, and thiamine became the first vitamin ever isolated from food. All because Eijkman looked up from his desk, open to finding answers in unexpected places.
3. Get out of the office.
Francisco Lopera was a young Colombian neurologist in the 1980s when he first saw a patient with early-onset Alzheimer’s disease. The man, only in his early 40s, had developed terrible memory loss. Lopera learned that the patient’s father and grandfather had suffered from the same disease at the same age. Lopera became so curious about the patient that he began traveling for hours by car, horse, and foot over cracked roads and overgrown paths to interview people in the patient’s extended family. He kept track of people on index cards, jotting down notes about each person’s symptoms and relatives, then arranging the cards back in his office to fill out the family tree. Over more than a decade, Lopera recreated an enormous family tree that he and a colleague traced back to European ancestors that had lived hundreds of years earlier, and probably carried a genetic mutation that caused early-onset Alzheimer’s disease.
“We often see our work as bounded by buildings and space, when in reality we can get more information if we are willing to explore beyond traditional settings.”
Today, the families make up one of the most important research cohorts in the world when it comes to finding a cure for Alzheimer’s disease. But they were only discovered because Lopera was enough of an out-of-the-box thinker to realize that his medical practice need not be limited to the exam room. We often see our work as bounded by buildings and space, when in reality we can get more information if we are willing to explore beyond traditional settings.
4. Choose what you want to know.
Nancy Wexler was a Fulbright scholar in her early 20s when she found out that her mother was dying of Huntington’s disease. Wexler learned that this gave her a 50 percent chance of getting the disease herself. She had essentially no training in biology at the time, but decided to devote her life to finding a cure for Huntington’s disease. She quickly understood that the first step was identifying the gene that causes the disease. So she overhauled her career and, along with her father, began organizing workshops that brought together scientists from different disciplines to talk about novel ways to find the Huntington’s gene. Eventually, these collaborations helped locate the gene on chromosome 4. The technology allowed doctors to perform predictive testing, so people could find out whether they carried the genetic abnormality that causes Huntington’s disease before they actually developed symptoms.
Wexler decided not to take the test herself. She felt that she enjoyed her life, and had more to lose from finding out that she carried the genetic change than she had to gain from finding out she didn’t. Decades after she discovered the gene, her limbs started to writhe in the typical way of Huntington’s disease, but she’s never voiced regrets over not getting the information earlier.
In my own clinic, we often talk to patients about genetic testing for conditions that have no proven treatment. There are a lot of factors that go into the decision: whether the results would help with planning for the future, if drugs trials are available, or someone in the family is having children soon and might use IVF to eliminate the mutation from their lineage.
“Before we seek answers, maybe we should ask, ‘What will I actually do with this information?’”
Ultimately, genetic testing is about a more commonplace question: how much information do we really want to know? Is all knowledge power? Can we be more thoughtful about what information we choose to acquire in news outlets, social media, and scientific journals? Before we seek answers, maybe we should ask, “What will I actually do with this information?”
5. Understand your diagnoses.
As a dementia doctor, the most common question I get from patients is, “What’s the difference between Alzheimer’s disease and dementia?” The words describe two separate things. Dementia describes how well you function in everyday life—in particular, that a person isn’t able to do complex activities like managing finances, cooking, or driving, because of difficulties with thinking. Alzheimer’s disease, on the other hand, describes what is going on in the brain at a microscopic level. Dr. Alois Alzheimer discovered these microscopic structures in a patient’s brain in the early 1900s: plaques (which looked sort of like spray-painted spots) and tangles (which look like strings of spaghetti) inside of neurons. Today, we know that plaques are made of a protein called “amyloid,” and tangles are made of a protein called “tau.” Alzheimer’s disease refers to the presence of amyloid and tau in the brain.
Alzheimer’s disease is the most common cause of dementia, but we have plenty of patients with dementia that’s caused by something other than Alzheimer’s disease. We also have patients who have normal memory and thinking even though their brains have amyloid and tau aggregates—so they have Alzheimer’s disease, but not dementia.
Dementia is hardly the only misunderstood medical diagnosis. Studies suggest that about 90 million Americans have low health literacy, and poor health literacy is associated with more frequent hospital stays and higher mortality. So, know your diagnoses. Ask your doctor if you aren’t sure what your diagnosis means, or how it affects you. Don’t be embarrassed to ask how to pronounce your medications, and what each of them is for. Even your doctors probably didn’t know how to pronounce the medications until they went to medical school.
To listen to the audio version read by author Sara Manning Peskin, download the Next Big Idea App today: