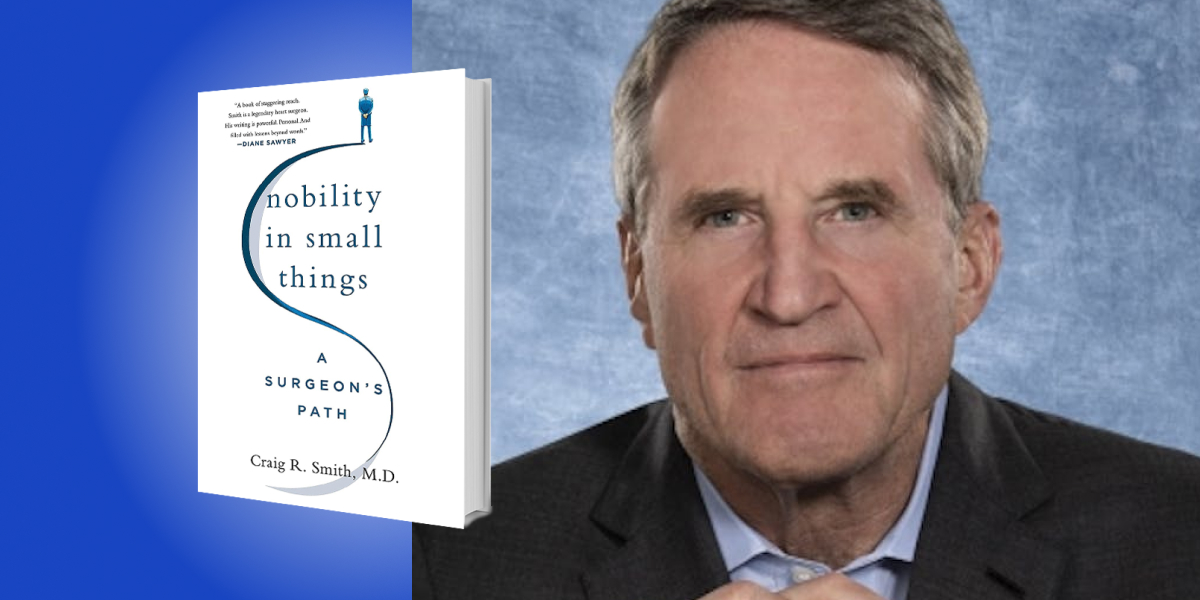
Craig Smith is the Chairman of the Department of Surgery at Columbia University and the New York Presbyterian Hospital. He was dubbed “The Pandemic’s Most Powerful Writer” by The Wall Street Journal during the Covid pandemic.
Below, Craig shares five key insights from his new book, Nobility in Small Things: A Surgeon’s Path. Listen to the audio version—read by Craig himself—in the Next Big Idea App.
1. Big events are defined by their uncertainty.
That might sound odd coming from someone with a strong background in science—isn’t science where we go to find certainty? Yes and no; theology might be a safer bet.
One of the biggest events in recent history started in late December 2019, when a few cases of a new coronavirus were detected in Wuhan, China. It was found to be closely related to SARS and MERS, neither of which had become pandemic. That bit of hopeful certainty was reassuring for a month or two until the shock of the COVID-19 pandemic became undeniable. “Follow the science!” became the battle cry, often with an air of desperation, evoking a world crumbling into anarchic chaos, and implying that science was being willfully ignored.
In truth, most of the science specifically relevant to the problems at hand simply didn’t exist. We had no map, no algorithm, no Bloomberg Box. On the fly, we were figuring out how to prevent, how to test, how to treat, creating the science in our wake. Much of it rested on epidemiology, which can take months or years to answer simple questions. At the beginning of the pandemic, everyone felt battered by conflicting and rapidly changing “truths” that were derived from incomplete data. Urgency skeletonized the normal processes of peer review, and oracles became self-proclaimed. The anxieties of the pandemic focused a huge new audience on how the sausage is made—an immersion crash course in the messy, imperfect, subjective, political, and fascinating nature of scientific evidence, revealing how bright lines drawn through murky grays created policies that changed every day.
Is that what we get in our hour of need, to see how science is so much like the rest of life? Desperation for answers created an intolerance of uncertainty at a time when the myth of certainty was never more obvious.
2. Professionalism includes accepting personal responsibility.
Professionalism is more than just doing your thing for money. Certain professions carry moral and ethical expectations, most obviously medicine and law, but also fields like financial services, engineering, and journalism. Those expectations have a common obligation to subordinate self-interest when one is acting in a professional capacity. The interests of patients, clients, customers, or readers come first. Those obligations accrue because membership in those professions is an earned privilege, and with privilege comes responsibility.
Responsibility is a term entangled with assignment of cause and effect, which is why espousing personal responsibility marks me as someone who hasn’t learned that all problems have systemic causes. I’m not presuming to challenge that simplistic notion for all human society. I’m narrowly focused on accepting personal responsibility for actions taken by surgeons like me. In something as complex as open-heart surgery, innumerable cause-and-effect relationships contribute to an outcome. Many are (to some degree) systemic, but my actions are mine alone, even though they interact with systems. Sometimes a bad outcome results from those actions for which I am solely responsible. What is that responsibility, if not personal?
“The acceptance of personal responsibility becomes a dangerous threat to a doctor’s ‘wellness.'”
Responsibility for a bad outcome is a difficult burden to bear, but it comes with the job. Suppose my financial planner makes a disastrous investment and I lose my savings, or my lawyer fails to pursue key evidence and I go to jail. I hope each of them will accept some personal responsibility for my bad outcome. I doubt either will expect their heavy emotional burdens to be my main concern. As my profession becomes preoccupied with personal burdens, the acceptance of personal responsibility becomes a dangerous threat to a doctor’s “wellness.” I fear we are throwing the professional baby out with the personal bathwater.
3. Where, oh where, has wellness gone?
Preserving the precious essence of “wellness” in doctors has become a high priority. That goal is newly enshrined in my medical school’s recent revision of the Hippocratic oath. Every department in the medical school has a Wellness Officer. Frequent survey questionnaires attempt to measure wellness, and its evil twin, burnout. The common stresses and aggravations of delivering health care in a complex urban medical center—long hours, untidy stairwells, slow elevators, crowded waiting rooms, delays on the A-train—now trigger an extra layer of alarms by constituting threats to our wellness. This bothers me for several reasons.
Wellness is not a goal, it’s a state of passage. Think of a transatlantic ocean liner leaving New York. If my goal is Europe, I’ll get there whether I stow away in the bilge or dine and dance in first class. If my destination is paramount, differences in my wellness during the passage matter very little. Contrast that to a ship that leaves Miami and returns to Miami after touring the Caribbean. The goal becomes the passage itself; the wellness gap between the bilge and first class is all that matters. I fear that my profession is losing sight of the destination and has shifted focus to the voyage. As a side effect of that shift in focus, the gratifications of hard work well done—of reaching the goal, arriving at the destination, no matter the journey—are discounted as contributions to positive wellness.
If I don’t meet my Wellness Officer’s definition of wellness, am I burned out? Wellness and burnout are not binary, like opposite faces of a coin. In my experience, it’s quite the opposite. Under the spacious skies, in the amber waves of grain, there are countless acres of wellness to be enjoyed between the borders of burnout and ecstasy.
4. Accuracy of performance assessment is directly related to workload.
During the first few months of my five-year general surgery residency, the Chairman of Surgery confided in his two Chief Residents that I would need to find another place to complete my training. He’d reached this conclusion based on one second-hand misrepresented event. The most competitive surgery residencies of that era were pyramidal. In my situation, that meant only three of the nine residents who started together would be invited to continue after the second year. My Chiefs had a different impression of my performance, and by the end of the first year, they’d changed the Chairman’s mind.
I’m forever grateful to my Chiefs for their advocacy, but it was not capricious, and we were not friends. I prevailed because so much was asked of me every day that a misimpression could not stand against the sheer volume of observation. And I was not unique—the same mass of performance data was accumulated by all my fellow residents. Someone will say “Of course you and your two buddies who survived the pyramid liked the process, but what do the other six think?” It’s possible they would say all that data became a self-fulfilling prophecy by supporting unfair first impressions. Against that I can only offer, after observing the process from an increasingly senior perspective over 45 more years, that it seems remarkably accurate, and supports my hypothesis: the more that’s expected of you, the harder it is to be misjudged.
“Your first day is harrowing enough without expecting perfection.”
Everyone’s heard the old saying “You only have one chance to make a first impression!” Lighten up! Your first day is harrowing enough without expecting perfection. If it’s a very demanding role, within a few weeks no one will remember that you stammered, blushed, and spilled coffee on the conference table.
5. Fanfare for the Common Man.
In Chicago, around 1962, my piano teacher took me to hear Aaron Copland conduct some of his own works, including Fanfare for the Common Man. I loved it, although I didn’t know much about common men. When I started working for a wage, I worked with common men every day. During summers in college I worked in a steel mill. The workforce was male, inner-city, majority Black, and high school educated at most. After dropping out of graduate school I worked as a telephone lineman in Vermont, where my fellow linemen were male, rural, white, and high school-educated. The work in both settings was hazardous, strenuous, physical labor. I was a comparatively over-educated male, and neither rural nor inner-city—but if I did the work, they had my back. They trained me, shared their tips and tricks, and cared when I was injured. They took pride in the skilled parts of their jobs. These common men worked hard for meager salaries, and many worked more than one job.
It would be hard to call my current role common, but I am surrounded and supported by common men and women. “Common” often implies uninteresting or pedestrian, leaning towards unimportant. The Boston Common is not pedestrian or unimportant. Never were the admirable connotations of “common” clearer than during the Covid pandemic. Many of the heroes in my hospital were personnel in the rarely celebrated ranks of housekeeping, transport, maintenance, and security. They were directly in the line of fire, shoulder to shoulder with everyone else, even when we had barely enough PPE to keep them safe. Unlike me and my ilk, that staff hadn’t attended fancy colleges and professional schools on the conveyor belt to large incomes. They were as stressed, short-staffed, and overworked as anyone in the hospital. But these common men and women kept showing up because they believed in doing their jobs. They were the dependable belly of the bell-shaped curve—the backbone that never broke.
To listen to the audio version read by author Craig Smith, download the Next Big Idea App today: