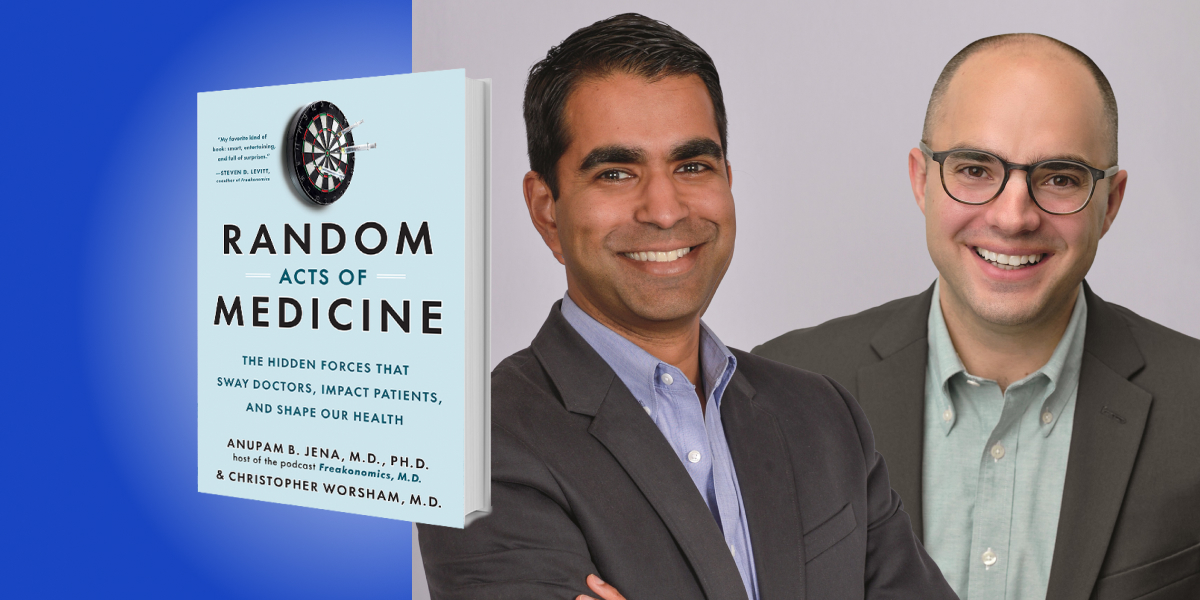
Apunam Jena, MD, Ph.D., is an economist, physician, and the Joseph P. Newhouse Professor at Harvard. Jena hosts the Freakonomics, MD podcast, which explores the hidden side of health care.
Christopher Worsham, MD, MPH, is a researcher, pulmonologist, and critical care physician at Harvard.
Jena and Worsham practice medicine at Massachusetts General Hospital. Their research and writing have been published by the New England Journal of Medicine, JAMA, New York Times, Wall Street Journal, and Washington Post.
Below, Anupam and Christopher share 5 key insights from their new book, Random Acts of Medicine: The Hidden Forces That Sway Doctors, Impact Patients, and Shape Our Health. Listen to the audio version—read by the authors—in the Next Big Idea App.
1. Chance affects every aspect of our lives, including our health, and we can learn from it.
Not too long ago, I met somebody who told me that they met their spouse at the DMV. You know that’s totally random because it’s not actionable. You would never tell your son or your daughter, “When you grow up, go to the DMV to meet your soul mate,” right? Chance occurrences like that affect us every day. In the context of medicine, you could have someone who is diagnosed with cancer who doesn’t have any risk factors, or who is hit by a car—both are totally random.
But there are ways in which we are exposed to random occurrences, by chance, that can teach us something almost like we’re part of a natural experiment.
Both of us have kids who were born in August, and that means we bring them in for their annual physicals in August. But every time we do that, the flu shot isn’t available. When we leave the doctor’s office, the pediatrician tells us to make sure we make an appointment in a couple of weeks to come back for a flu shot, because the flu shot isn’t available until September or October.
That’s a real pain to have to come back and it makes you wonder: what if our kids happened to have been born just a month later in September? If they had been born in September, would they be able to get their flu shot when they came in for their annual visit? It makes us wonder if this goes beyond just our kids. Any kid born in the fall is going to have an easier time getting the flu shot than kids born at other times of the year.
It turns out, in a study that we did, about 55 percent of kids who happened to be born in October got their flu shots versus just over 40 percent of kids born in, say, June. In turn, the kids born in June were more likely to get the flu. A random characteristic, such as the month someone was born, was leading to differences in health outcomes for these kids. It also told us that logistics—having to come back for another appointment—ended up really mattering.
2. In healthcare, less might be more.
It’s easy to think that more medical care is getting better. It has gotten better at searching for more cancers, unclogging more arteries, or treating more diseases. But the data tell us that more isn’t always better, and sometimes, less is more. Here’s a quick example from 40 years ago.
When Israeli physicians were negotiating a contract with the government, they went on strike. During that strike, they only made essential medical services available. During that time, mortality for patients living in the area stayed the same. It was the same as it was just before the strike and just after the strike. It was the same as it was during that same time period the year before. So, in Israel, we saw that having less medical care didn’t actually seem to result in any more patients dying.
“If you happen to have a cardiac arrest during the dates of one of these major cardiology conferences, when all the cardiologists are out of town, the mortality rate falls to 60 percent.”
Another example of less is more took place while working as a resident training to be a doctor. I (Apunam) happened to be in the cardiac intensive care unit during the dates when there was a major cardiology conference occurring in the country. These two conferences are for the American Heart Association and the American College of Cardiology. I wondered whether or not the outcomes of patients with cardiac problems might be worse because of this reduction in staffing—or what I perceived to be a reduction or a change in staffing. Some colleagues and I looked at it, and we found the complete opposite: we actually found that people did better.
Here are some of the numbers; If you have something called cardiac arrest, which is when your heart stops, 70 percent of people with that condition who make it to the hospital are actually dead within 30 days, so it’s extraordinarily high risk. If you happen to have a cardiac arrest during the dates of one of these major cardiology conferences, when all the cardiologists are out of town, the mortality rate falls to 60 percent. That’s huge—you take the effect of cholesterol medications, blood pressure medications, stenting of the heart, and put it all together, it doesn’t deliver that same level of benefit.
The other data point that we found was that the rate of a very important cardiac procedure fell by about 30 percent, so it was happening less often. The intensity of care during the dates of those meetings was lower, and there are a lot of reasons why that might be true. But the take-home point was that in a scenario of doing less for patients with cardiac disease or acute cardiac disease, we actually observed better outcomes and lower mortality.
That speaks to this idea of how data applied in a creative way can tell you that sometimes more is more and sometimes, less is more.
3. We can’t do randomized studies where we knowingly expose people to harm just to see how harmful something is.
That would be unethical. But when people are exposed to things that we think might be harmful by chance, we can learn from it by looking at the data in the right way. There’s this one axiom that is common in emergency medicine, and acute care in general, about heart attacks. In these scenarios, we say that “time is tissue,” meaning that the longer it takes to treat someone with a heart attack, the more damage gets done to the heart muscle. But is there a way we can measure just how much those minutes count?
There is, and actually, the question being asked is really fundamental. As a doctor or a nurse, or even as a patient or a person with a medical problem, one of the biggest questions we’ve got to ask ourselves is, “How quickly do we need to act?” If you’re a nurse or a doctor in the hospital and someone’s short of breath, do you have minutes? Do you have hours? Do you have days to sort it out? If you’re a parent at home with your kid who has a fever and a headache in the middle of the night, do you have to call the pediatrician right then? Can you wait until the morning? What do you do?
The only way you would figure this out is if you actually randomize people to get care for chest pain immediately or wait 30 minutes or two hours, which would be unethical. But we found a way to try to get at this question of how much minutes matter by looking at this natural experiment from marathons. A few years ago, my wife was running a race. It was in Boston, and she wanted me to watch her on the race route. It happened to pass near the hospital where I work, and so I was going to park at the hospital and watch her. But when I was trying to get to the hospital, the road was blocked because of the race. Hours later, my wife asked, “Well, what happened to everybody who needed to get to the hospital that day?” That sparked an idea for how we could look at this question.
“On the date of a marathon, the mortality rate for people who live along the marathon route goes up about 20 percent.”
We started looking at what happens when cities host marathons. On the date of a marathon, the mortality rate for people who live along the marathon route goes up about 20 percent. Keep in mind that these are older Americans, not people who are running the marathon. We show that the reason it goes up is that there’s a delay in ambulance transport times; it takes longer for people to get to the hospital and thus people are more likely to die. What we show is just on the order of minutes. This was a way that we could use this natural experiment, a major marathon, to show that minutes really do matter when it comes to outcomes.
If you want to figure out this question in another way, you could look at people who got care quickly and looked at people who delayed their care. Let’s say you found that people who delayed their care on purpose had worse outcomes. That’s not a good way to answer that question, because people who delay their care are different in a lot of other ways. You don’t know if it’s the delaying care that led to a bad outcome, or if it’s everything else about those people that’s correlated with their decision to delay care which led to the bad outcome. The marathon variable was an example of a natural experiment being able to answer the question of how quickly we need to act when it comes to our health.
4. We don’t actually know exactly what makes a good doctor.
Let’s say you’re a patient, and you walk into a room and see a doctor come into the room who looks young. Would you be worried, would you rather that that doctor had more gray hair and had more experience? How would you feel if the doctor was a man or a woman? Or if they had gone to Harvard Medical School, or attended medical school in this country versus outside of this country? All of those things are things that we probably think a lot about, but we don’t have much good evidence in this respect. This brings us to another basic question in medicine, which is: Does the experience of the doctor that you see matter?
There aren’t a lot of great ways to answer this question. The reason for that is because, while looking for a new doctor, I might search for a doctor who’s my age; while someone who’s older than me might search for a doctor who’s older. That’s not random. Therefore, we can’t look at someone like me who gets sick and seeks out a younger doctor, and then when I do, say that younger doctors are better. We have to find a situation where doctors are getting assigned randomly to patients.
That actually happens quite frequently in the hospital. These days, patients get assigned to an internal medicine doctor called a hospitalist, and they are assigned to whichever hospitalist happens to be on duty. It’s a nice randomizing event. In a study we did with some colleagues, we simply asked what happened to patients based on how old the hospitalist was who admitted them. What we found was that as the hospitalists got older, the mortality of the patients they admitted to the hospital went up. At first blush, it makes you think, “I definitely don’t want to be admitted to an older doctor if that’s the case.” But digging a little deeper, the data also showed that doctors who were older but continued to see a lot of patients stayed sharper since they were seeing more patients continually. Their patients did just as well as the patients who were seen by younger hospitalists.
At the end of the day, the question shouldn’t be, “Do I want a more seasoned doctor with gray hair?” The question should be “How many patients is this doctor seeing on a regular basis in order to stay sharp?”
5. Behavioral economics isn’t just fodder for consumer advertisers; it shows up in high-stakes situations, too.
If you go to the grocery store and you see a bag of chips that costs $1.99, maybe you wonder why it’s $1.99 instead of $2.00. The reason is because of something called left digit bias. It’s the tendency of the mind to focus on the leftmost digit in a string of numbers. Something that’s $1.99 feels something like $1.00 and something that $2.00 feels like it’s $2.00, and $1.00 is less than $2.00.
“The older the patients, the less likely doctors want to do something aggressive with them.”
What does it have to do with medicine and our healthcare? We did a study a while ago in which we looked at people who were admitted to the hospital with a heart attack. One of the things that you can do to treat a heart attack is do a cardiac bypass surgery. What we saw was that people who happened to come to the hospital when they were 79 years old and 50 weeks—just about to turn 80—were more likely to receive a cardiac bypass surgery than someone who happened to come to the hospital with a heart attack just a couple of weeks later, when they were 80 years old or more. The reason is that the older the patients, the less likely doctors want to do something aggressive with them. For someone who’s 80 years old and one week, they feel like they’re “in their 80s,” and for someone who’s 79 years old and 50 weeks, they feel like they’re “in their 70s.” That’s the intuition.
The other thing that we found is that the mortality rate at one year was basically the same in these two groups. We had a bunch of people who were 79 years and 50 weeks old, who were more likely to get a cardiac bypass surgery. But one year after that decision, they were no more likely to be alive as a result of that surgery. This speaks again to the idea that sometimes, less might be more.
When we think about behavioral economics, we often apply it to decisions that people make that aren’t high stakes. Sometimes the studies that support behavioral ideas come from very controlled settings, like in a laboratory, where the stakes aren’t high. But in a medical situation with a complex cardiac procedure, people are really, really sick. In that setting, a heuristic can operate—no pun intended—in the back of a physician’s mind and make them do something that they might not otherwise do if they were aware of that bias.
To listen to the audio version read by co-authors Anupam Jena and Christopher Worsham, download the Next Big Idea App today: