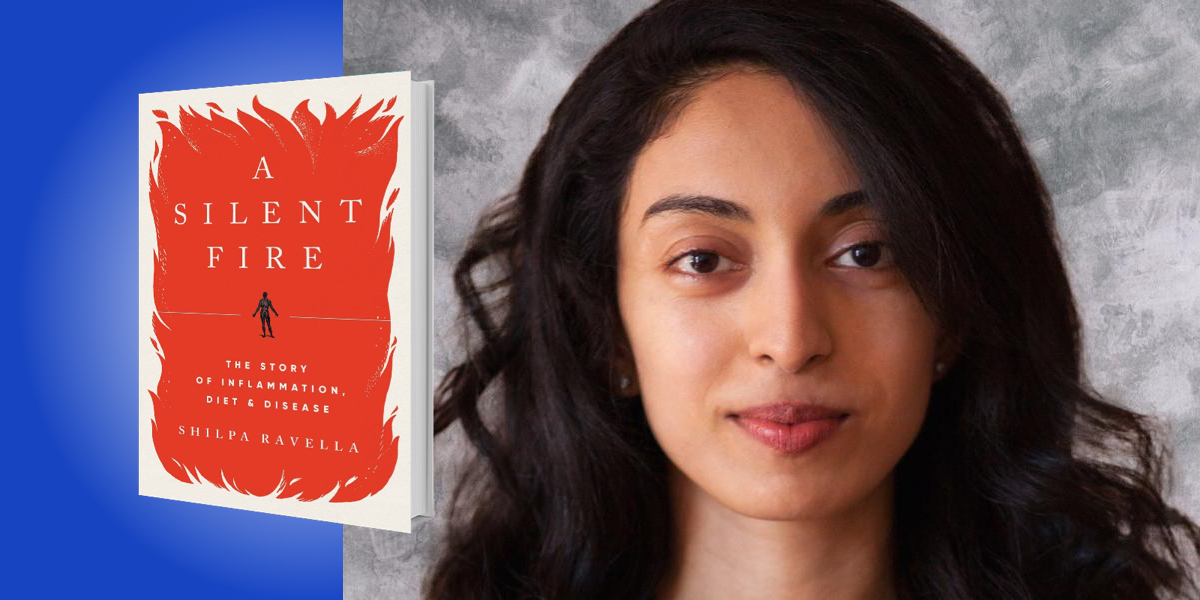
Shilpa Ravella is a gastroenterologist with a specialization in nutrition. She has unique experience in treating rare digestive ailments such as intestinal failure and multiple-organ transplantation.
Below, Shilpa shares 5 key insights from her new book, A Silent Fire: The Story of Inflammation, Diet, and Disease. Listen to the audio version—read by Shilpa herself—in the Next Big Idea App.
1. Inflammation has a fundamental role in nearly all modern chronic diseases.
In its ancient role, inflammation is a benevolent force that evolved to fight infectious germs, poisons, and traumas, all of which humans routinely succumbed to. When you cut your finger or stub your toe, you see the cardinal signs of inflammation working to heal the wound: redness, heat, swelling, and pain. Blood flow quickens as arteries and veins dilate, and fluid and protein leak out into tissues. But inflammation is not always helpful. For instance, the visible inflammation in autoimmune diseases like rheumatoid arthritis or lupus, in which joints swell and rashes erupt.
We’re finding that the dark side of inflammation is more pervasive than ever imagined, extending beyond typical autoimmune diseases. Low-level inflammation, or hidden inflammation, is rarely tested for or treated, but it is tied to many chronic diseases, including heart disease and cancer. In fact, it may be a common thread running through nearly all disease, like obesity, diabetes, neurodegenerative and psychiatric disorders, and even aging itself. This type of inflammation proceeds insidiously: it floats in our bodies unheeded, unseen and unfelt, until one day it wreaks havoc.
In the 21st century, we’ve reached a tipping point. We can now say that inflammation is both a consequence of disease and potentially a root cause. Low-level, hidden inflammation has even gained traction in the medical literature as we increasingly understand it as a silent killer.
“We can now say that inflammation is both a consequence of disease and potentially a root cause.”
The idea that hidden inflammation may be a shared biological mechanism between distinct diseases fosters a new understanding of human health. It compels us to consider treating diseases in concert, taking into account the totality of the patient’s health as conditions interact.
2. The ties between inflammation and our microbiomes.
We have trillions of bacteria, viruses, fungi, and protozoa teeming on, in, and around us. Human intestines are home to more microbes than any other part of the body. This gut microbiome is crucial for health. It functions like a vital organ, with a metabolic capacity that surpasses that of the liver.
The microbes in the gut have a variety of important functions. They ferment what we cannot digest, harvesting energy. They degrade toxic substances. They protect against deadly germs. And we’re now also realizing that gut microbes play a central role in immune function and inflammation. The microbes in our intestines have conversations with immune cells in our gut and beyond at all hours of the day. They help shape the immune system.
For example, if you look at germ-free mice, which are delivered by C-section, grow up in plastic bubbles, and subsist on sterilized food and water, these mice face major problems, like deformed hearts, lungs, and intestines, brain defects, and maladjusted immune systems that cannot defend against germs yet readily attack the body’s own tissues. The conversations between microbes and immune cells both shape the immune system and are shaped by the immune system.
“The microbes in our intestines have conversations with immune cells in our gut and beyond at all hours of the day.”
This intricate dialogue is how our bodies are trained to distinguish harmless food and germs from toxic counterparts. It affects things like succumbing to a deadly infection, getting seasonal allergies, or failing to build immunity after a vaccine. It also affects the risk of developing hidden inflammation. We need exposure to the right quantity and quality of germs to foster these essential conversations and create an optimal inflammatory state and an immune system that reacts accordingly to challenges.
3. Diet can dictate inflammation.
A growing body of research supports the power of diet in causing, preventing, or treating inflammation—and there is indeed such a thing as an anti-inflammatory diet. But defining an anti-inflammatory diet gets complicated. How do you define this diet when eating itself is an inflammatory act? All meals incite a flash of inflammation, to varying degrees. In fact, scientists once wondered if the mere digestion of food is a type of infection.
We need to make a distinction between the physiologic inflammation triggered by food and the excessive, persistent inflammation (often low-level) which is triggered by long-term eating patterns and environmental factors, because it’s the latter type of inflammation that leads to chronic inflammatory diseases. To figure out the anti-inflammatory diet, we need to consider how food affects our microbiomes and look at the gamut of nutrition science from both a historical and evolutionary perspective.
4. Understanding the intricate interactions between hidden inflammation, food, and germs can help us adapt to our current environment.
Humans were designed to survive and reproduce amid killers like infections and traumas, so we evolved bodies capable of robust inflammatory responses. In this historical setting, the cost of provoking an inflammatory response was usually a reasonable price to pay, but today’s human environment is transformed. Without constant, life-threatening infections and other dangers, the cost of a robust or even a low-level inflammatory response is higher. Modern immune systems are incredibly sensitive to triggers, and we don’t see or feel the price of constant, low-level stimulation of the immune system until years or decades down the line. At the heart of hidden inflammation is an incongruity between the ecological niche we evolved to inhabit and the one most of us currently occupy.
“The similarities between a diet for planetary health and one that manages inflammation are striking.”
Our current environment is plagued by chronic diseases, climate change, and global pandemics. Hidden inflammation can help explain why ostensibly healthy people may succumb to severe illness during epidemics and pandemics. It weakens immunity, predisposing us to infections. It also increases the likelihood that our immune systems will mount an overwhelming, inappropriate attack against germs, leading to unfavorable outcomes. Regarding climate change, the links between human and planetary health are inextricable, and one of the best weapons against the destruction of the planet is to change the way food is produced and consumed. The similarities between a diet for planetary health and one that manages inflammation are striking.
A positive aspect of our current environment is the unprecedented potential of the modern world to maximize health and longevity. As human lifespans increase, each of us are more likely to require modern medical interventions that warrant immune manipulation—from advanced prosthetics to organ transplants to cancer immunotherapy. We are new humans, comprised of new materials, and controlling inflammation through lifestyle changes—which is a form of gene therapy—will help us survive and thrive in this new context of human life.
5. Inflammation is omnipresent in sickness and health.
Most of us suffer one or more chronic inflammatory diseases. Nearly every medical practitioner encounters inflammation in some form, addressing it piecemeal from the vantage point of various specialties. We are all bound in this struggle for balance: an attempt to capture inflammatory equilibrium.
Despite the insidious side of inflammation, the story of how we came to define this entity and how we interact with it, is also rich and protracted. This story is at once old and new. It’s a story grounded in history and hard science, and it celebrates the scientists dedicated to shedding light on this grand puzzle.
Hidden inflammation is a cause of disease, but we have the tools to prevent it, treat it, and in effect, optimize human and planetary health.
To listen to the audio version read by author Shilpa Ravella, download the Next Big Idea App today: