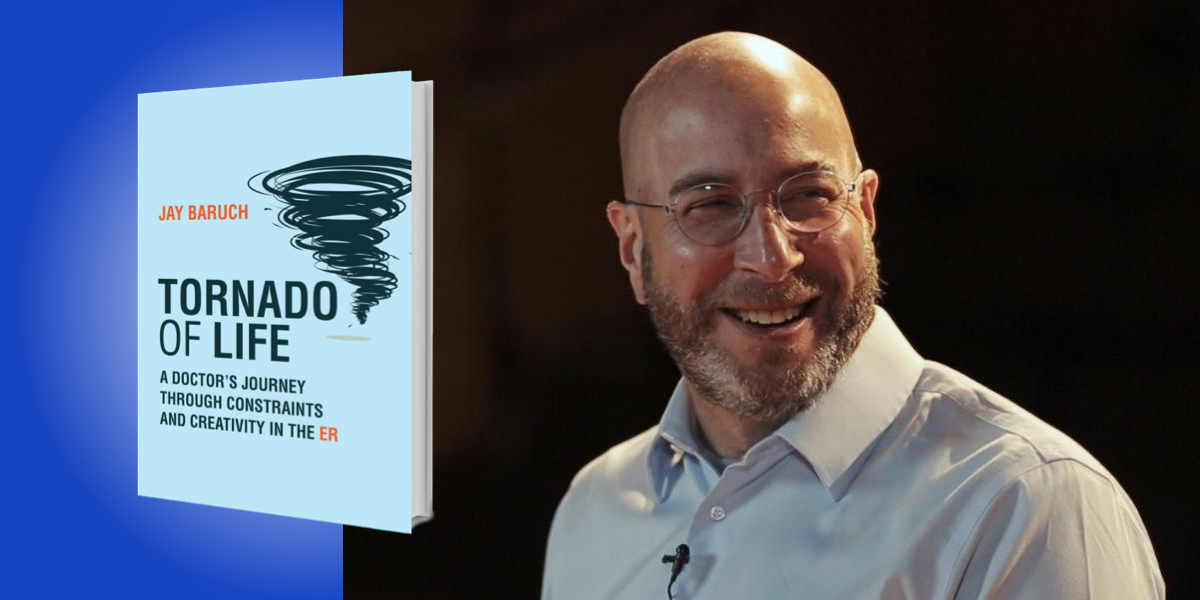
Jay Baruch is a practicing emergency room physician and Professor of Emergency Medicine at Alpert Medical School of Brown University, where he directs the Medical Humanities and Bioethics Scholarly Concentration.
Below, Jay shares 5 key insights from his new book, Tornado of Life: A Doctor’s Journey Through Constraints and Creativity in the ER. Listen to the audio version—read by Jay himself—in the Next Big Idea App.
1. People are their stories, not data with faces.
In the narrative disaster zone of the ER, my primary focus is making sure the story the patient is telling is the one I’m hearing. In a fast-paced environment, a provider faces unprecedented challenges while burdened with mounting constraints. But every patient deserves to feel heard.
Patients are challenged with a daunting task: construct a deeply personal story and confide in a healthcare provider, who, until that moment, was a stranger. I am unable to care for patients without caring for their unique stories.
The narrative scholar Kathryn Montgomery voiced this challenge beautifully: “Clinicians work to perfect the maps of illness, but each patient, each instance of illness, is unchartered territory.” In medicine, evidence from rigorous research studies informs clinical decisions. Getting to the heart of a patient’s problems or needs, however, means listening to their symptoms while also being alert to less-obvious social and psychological burdens. This becomes easier when focusing on the anatomy of great stories, which center fascinating characters with desires and expectations, who then encounter troubles or obstacles. Patients are the writers and characters in profound stories of living a life. The problems of the body are often complicated by a slew of other problems, like relationships, money, mental health, substance abuse, and loneliness.
The cognitive psychologist Jerome Bruner said narrative is an “invitation to problem finding, not a lesson in problem solving. It is deeply about plight, about the road rather than the inn to which it leads.” That road may take me into unchartered territory, but healthcare providers must be willing and prepared to go there. The linguistic lineage of the word “emergency” dates to the Latin word which means “to bring to light.” Patients come to the ER for a myriad of reasons, but every patient has a story that needs to be told.
2. Uncertainty is our ally.
Uncertainty is everywhere in doctoring, from diagnosis and prognosis to communication. Uncertainty, however, doesn’t always feel good. To alleviate those feelings, we reach for more data, which usually means more diagnostic testing. However, I learned with my patient Jill L. that more data doesn’t promise more certainty.
“If we don’t welcome uncertainty, we might narrow the type of problems for consideration, limit what we’re listening for, or value only those details that support our preconceived beliefs.”
Jill L. presented one Saturday night with vague symptoms that included chest pain and shortness of breath, so I searched for problems that included a possible heart attack or a blood clot in her lungs. I was a young physician, diligent, courteous, and devoid of imagination. Unfortunately, I was so focused on “what” that I never asked “why?” Eventually, she told me why she came to the ER—she was a victim of interpersonal violence. The night that she came in, she had finally had enough and didn’t know where else to turn.
Studies have shown that physicians that are uncomfortable with uncertainty are prone to excessive diagnostic testing and they are less likely to include uncertainty in conversations with their patients. Excluding uncertainty in the conversation can cause psychological distress. The poet Mark Doty said, “It’s not always easy to remember that, in any process of inquiry, our uncertainty is our ally.”
Becoming comfortable with uncertainty requires changing our relationship with it. We shouldn’t ignore it, pretend it’s not there, or tailor our problem solving to questions with answers. If we don’t welcome uncertainty, we might narrow the type of problems for consideration, limit what we’re listening for, or value only those details that support our preconceived beliefs. It isn’t enough to tolerate uncertainty. We must learn to leverage and take advantage of uncertainty as markers for further investigation.
3. The remedy for uncertainty is not-knowing.
Becoming comfortable with uncertainty is aided by embracing the importance of not-knowing. I borrowed this notion of “not-knowing” from the writer Donald Barthelme’s essay of the same name. Barthelme describes the act of writing, and the creative arts in general, as a process of dealing with not-knowing. Problems are crucial to not-knowing. Without problems, there would be no invention.
Developing comfort with uncertainty and not-knowing is hard when physicians are incentivized for having the answers, not for owning up to what they don’t know. Not-knowing is a muscle that can become stronger and stabilized through training and interrogation of our thinking process, starting with the decisions we make even before we think we’re making decisions.
We can’t forget that we seek out information, it doesn’t choose us. For example, why do I select specific details to focus on in a patient’s story—or any story— like chest pain and difficulty breathing in Jill L’s case? What other details am I not focusing on? With Jill L, I felt stuck. Being stuck in medicine can imply failure, but through the lens of not-knowing, we welcome being stuck. It might be our clue to slow down and think differently.
“Developing comfort with uncertainty and not-knowing is hard when physicians are incentivized for having the answers, not for owning up to what they don’t know.”
How do we recognize when something is amiss, that we need to change gears and examine a situation through different eyes? For me, it starts with a feeling, a pressure that resembles when a story I’m writing feels disorganized. I find myself pushing it forward; forcing it. I’ve since learned to step back. The solution to “what next?” starts with a deep breath and the question; How did I get here, and why? Where’s the tension? What don’t I know? The invitation to interrogate our thinking process is more likely to occur in institutional cultures that value a willingness to take on problems.
4. The best medicine will not work on the wrong story.
As an emergency physician, I’m a professional story-listener caring for a pressured storyteller under stressful conditions. Stories aren’t always solid, complete entities exchanged between patients and clinicians. Instead, they often feel like first drafts. Not infrequently, suboptimal outcomes or miscommunication result from intelligent people who simply got the story wrong.
It’s hard to create stories. It’s not easy to put language to tender, complicated, and embarrassing experiences and share them with strangers even under ideal circumstances. Imagine you’re a patient: anxious, tired, trying to be understood, and terrified of what it might mean.
When writing sentences, you develop a different relationship to language. Not only are you aware of what’s been said and how it was phrased, but you also start to notice what is left unsaid, the critical silences or evasions that might contain the very thing you need to hear but is unsayable. Anna Deavere Smith wrote, “We can learn a lot about a person in the very moment that language fails them.”
Our brain craves narrative coherence. Experts from Daniel Kahneman to Jonathan Gottschall write about how we’re hardwired to take cognitive shortcuts. Unconsciously, we weave random, incomplete data into a story. We must be careful. Our mind is susceptible to creating a story that is different from the one the patient is trying to tell.
Modern medicine, with its fascination with technology, often ignores the power of stories. It won’t tell us when our questions and thinking are off the mark. The best medicine won’t work on the wrong story.
5. How we respond to constraints says a lot about us.
Years ago, an esteemed professor of medicine offered this remark after I gave a talk at his medical school: “You’re an ER doc. You don’t have time for story.” And he’s right. There are many constraints, and they’ve been amplified due to the unprecedented pandemic pressures.
Obvious constraints include lack of time, constant interruptions, being forced to make decisions based on incomplete information, and crowding. There are other less explicit constraints also, like emotional exhaustion, limits in compassion, and accommodating a healthcare system that seems to have forgotten that patients come first.
“Stories serve as portals of social interaction that pipe us emotionally into the experience of another.”
These constraints won’t stop patients from bringing their stories to the ER, I told the professor. In fact, these constraints serve as an argument for bringing as many tools as possible to these pressured spaces. Since that talk years ago, the pressure of spending less time with more patients has spread to other medical fields.
Stories reveal how people cope, succumb, and surmount the obstacles in their lives and make their way in a world we all share. Stories serve as portals of social interaction that pipe us emotionally into the experience of another. The pandemic has revealed that preparedness requires everyone—in healthcare and in society—to be adaptable, flexible, and creative. This starts with a willingness to understand the unchartered experiences of others. That can’t happen unless we recognize the constraints in our own thinking. We must lower our guard, draw up our courage, and invite people into our lives, even if it’s only a few steps. When others slowly creak that door open, we must find the courage to take those steps ourselves.
How we respond to constraints reveals something about us.
If I’ve learned anything in my three decades as a professional listener and storyteller, in the ER, and on the page, it is the importance of humility. It’s not always easy to understand another human, but it’s possible and necessary. We’re not going to be perfect, but making the effort matters.
To listen to the audio version read by author Jay Baruch, download the Next Big Idea App today: