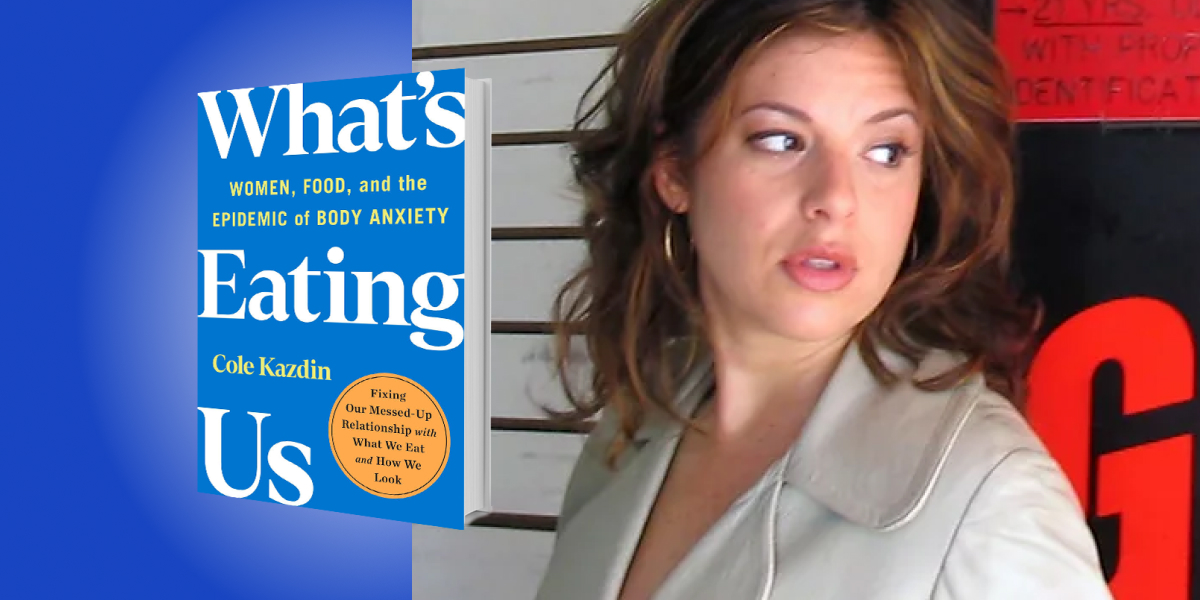
Cole Kazdin is a graduate from Northwestern University and Columbia University Graduate School of Journalism. She is now an Emmy award-winning television journalist and writer.
Below, Cole shares 5 key insights from her new book, What’s Eating Us: Women, Food, and the Epidemic of Body Anxiety. Listen to the audio version—read by Cole herself—in the Next Big Idea App.
1. We are all living in the midst of a deadly eating disorder crisis.
Eating disorders in the US have among the highest mortality rates of any mental illness; it’s on par with the opioid crisis. This is a surprising statistic because we don’t talk about eating disorders as a crisis in the same way we talk about opioid overdose.
About 30 million Americans will have an eating disorder in their lifetime. Most people are familiar with anorexia, which involves, among other things, extreme food restriction and starving, or bulimia, binging food and purging. However, most people who have eating disorders don’t fall neatly into one of those two categories. They sit somewhere else along the continuum of harmful behaviors around food and are still at just as high a risk for life-threatening health complications. During the pandemic, the number of people with eating disorders skyrocketed, especially teenagers, and the already-strained mental health care system is not equipped to handle it.
2. There is no standard of care.
There really is no standard of care for eating disorders. What this means is that there is no accepted, agreed-upon, proper treatment for eating disorders the way there is with other conditions. For example, if a person is diagnosed with Type 2 diabetes, there are medications to support this condition, like insulin, and a doctor may prescribe lifestyle changes, like increasing physical activity.
“It’s like the Wild West of medicine.”
It’s unimaginable that someone diagnosed with diabetes or schizophrenia, or another condition, could be prescribed riding horses, painting watercolors, or practicing some therapy that the doctor just invented. This is exactly what happens with eating disorders all the time. It’s like the Wild West of medicine. Part of it is because the field is not well-regulated, and it’s primarily focused on profit. It’s not that promising, evidence-based therapies don’t exist, but the onus is on the patient to track them down and vet them. The patient themselves needs to do research and evaluate, and in many cases, pay for it out of pocket.
3. We are all swimming in diet culture.
Diet culture is in the air we breathe. Reminders that we’re not thin enough or toned enough or healthy enough are everywhere, and we barely notice half of them. Ads on the radio and social media, labels on food in the grocery store—there’s even low-carb cat food at pet stores. When you ask a vet about it, they shake their head in disbelief; cats don’t need low-carb food.
The ubiquity of these messages may not even matter, as most of us have internalized it all anyway. Many behaviors that are genuinely harmful to the body have been rebranded. We’ve been so exhausted from the lack of carbs that we haven’t even noticed. “Fasting” and “intermittent fasting” are the new terms for “skipping meals” and “starving.” “Detox tea” has replaced “diuretics,” though they’re the same thing; “cheat day” used to be a binge.
“Many behaviors that are genuinely harmful to the body have been rebranded.”
The words “health” and “weight” have somehow become synonyms; “getting healthy” has become code for “losing weight.” Restricting food and limiting our calories, however, has nothing to do with health. In fact, according to one of the largest studies on the subject, dieting may increase the risk of developing an eating disorder.
4. Recovery is possible.
So is recovery really possible? Researchers at a leading institution would say so; communities of women are on the other side of their own eating disorders. These women are making it their mission, not only to create awareness but to help those not getting proper care.
Over time it is possible to learn the skills to overcome an eating disorder, learn new ways to manage anxiety, and learn to stop that daily analysis of the prior day’s eating and exercise. Recovery isn’t a straight line; it can look different for each person. It can take a long time, but it can absolutely happen. Eventually, one day, you might wake up, prepare your coffee and realize that your diet is no longer the first thing you think about.
5. Build community.
Building community is how we maintain recovery because it’s really hard to do without other people. It doesn’t mean you need to belong to some special group. Your community could be one other person, a friend, a partner, a family member, a clergy, or a group you find on social media. It doesn’t have to be a special eating disorder recovery group, although that can be helpful as we untangle and un-program all of the habits that we may have accumulated over the years.
It’s easy to underestimate the mental toll of even the most seemingly innocuous food rules we make for ourselves. If we think of stress as a sort of a fifth food group in terms of what we regulate for our health, it could serve us well. One researcher stated that if he had to pick one thing that we could do to improve our immune health, it wouldn’t be changing the way we eat or even adding physical activity, it would be finding new ways to manage stress. Finding other people to support us in that, and people that we can offer support to, makes all the difference in the world.
To listen to the audio version read by author Cole Kazdin, download the Next Big Idea App today: